Dermatology
Plastic, Reconstructive & Cosmetic Surgery
Our skilled team of Dermatologists and Plastic Surgeons provides personalized care using the latest techniques to enhance your appearance and boost your confidence.
Dermatology and Cosmetology focus on treating a wide range of skin concerns—from acne, uneven skin tone, and rosacea to more serious conditions like skin cancer, psoriasis, and eczema. Whether the problem is mild or complex, our dermatologists are experts in diagnosing and treating all types of skin conditions with care and precision.
Plastic, Reconstructive, and Cosmetic Surgery aims to improve or restore the form and function of body parts affected by birth defects, injuries, or medical conditions. The main objective is to help patients regain both confidence and physical function.
For emergency, chat with us.
+918287739641

our Services
Face Rejuvenation
Our facial enhancement services include Face Lift, Neck Lift, Rhinoplasty, Lip Augmentation and Reduction, Chin Augmentation and Reduction, Cheek, Jaw & Chin Implants, as well as Otoplasty (Ear Reshaping).
Breast / Chest
Our breast surgery services include Breast Augmentation, Breast Reduction Surgery, Breast Lift (Mastopexy), and Male Breast Reduction (Gynaecomastia).
Body Contouring
Our body contouring and sculpting services include Liposuction, Abdominoplasty (Tummy Tuck), Brachioplasty (Arm Lift), Medial Thigh Plasty, and combined Lateral Thigh Lift & Buttock Lift.
Other Procedures
Our aesthetic and restorative procedures include Fat Transfer, Ear Lobe Repair, Xanthelasma removal, Dimple Creation Surgery, Mole Removal, Hymenoplasty, Vaginal Tightening, and Hair Transplant.
Reconstructive Surgery
Our reconstructive surgery services include Cleft Lip & Palate repair, Ear Reconstruction, and Breast Reconstruction.
Comprehensive Care for Every Type of Cancer

Breast Cancer
What is the breast? Where is it located?
What is breast cancer?
Why have I developed breast cancer?
What are the symptoms of breast cancer?
Breast cancer can show up in different ways. If you notice any of the following changes, it’s important to see a doctor:
A sudden change in the size of one breast
A lump in the breast
Thickened skin or a sore that doesn’t heal
Redness on the breast
Discharge from the nipple
Nipple turning inward
Skin puckering or dimpling, especially when raising your arms
A lump in the underarm area
Any new or unusual change in the breast
In western countries, regular screening is common because breast cancer is more frequent. Women aged 40 to 50 and above are usually advised to get a mammogram every one or two years. In India, we don’t have a nationwide screening program, but women over 40 — especially those with a family history of breast cancer — should get a mammogram as a starting point. After that, your doctor can guide you on how often it should be done.
What investigations will I be subjected to?
To find out if someone has breast cancer, doctors may use different tests like a physical check-up, mammogram, ultrasound, or MRI. If they see something unusual, they might do a biopsy to look at the tissue closely. These tests help the doctor understand the type of cancer, how big it is, and how far it has spread.
Are there different types of breast cancer?
At what stage is the cancer?
Now that I have been diagnosed to have breast cancer, how will I be treated?
There are different treatments available for breast cancer, and the choice depends on the stage and type of cancer. Most patients need surgery unless the cancer has already spread to other parts of the body. Along with surgery, doctors may use one or more of the following treatments:
Surgery – removes the cancer from the breast
Chemotherapy – uses strong medicines to kill cancer cells or stop them from growing
Targeted Therapy – uses drugs that attack only the cancer cells and not the healthy ones
Radiotherapy – uses X-rays or light to stop the cancer from coming back in the same area
Hormone Therapy – given as tablets for 5 to 10 years to patients whose cancer grows with hormones (ER/PR positive)
Bisphosphonate Therapy – an injection (zoledronic acid) given every six months for three years, usually to post-menopausal women, to protect bones and also help in breast cancer treatment
Some patients may get chemotherapy or targeted therapy after surgery to make sure any leftover cancer cells are destroyed. Each treatment is chosen carefully based on what suits the patient best.
What kind of surgery is done for breast cancer?
Types of Surgery for Breast Cancer
Surgery for breast cancer usually includes two parts: surgery for the breast and surgery for the axilla (underarm lymph nodes).
Breast Surgery
Breast-conserving surgery, also known as lumpectomy, is done when the tumor is small and in the right area. The surgeon removes only the cancer, and the rest of the breast is saved. This depends on the tumor size, breast size, number of tumors, and cancer stage. If this option is possible, it is a safe and effective treatment. However, radiation therapy is always needed after this type of surgery.
A mastectomy means removing the whole breast. This is done when saving the breast is not possible, or the patient prefers to have it removed. The skin is closed neatly after surgery, and a straight scar is left without any open wound.
Oncoplastic is done when a large amount of breast tissue has to be removed. In such cases, nearby fat or tissue (like from the back or side) is used to fill the gap and improve the breast’s shape.
Breast reconstruction is an option to rebuild the breast after mastectomy. It can be done using the patient’s own tissue, usually from the tummy, or with a silicone implant. This can be done during the first surgery or later.
Axillary (Underarm) Surgery
Surgery for the lymph nodes in the underarm is part of breast cancer treatment. If it is done during a mastectomy, there is no extra scar. If it is done with breast-conserving surgery, there might be a small scar in the armpit area.
A sentinel lymph node biopsy is done to check the first set of lymph nodes that drain from the breast. These are removed and tested during surgery. If cancer is found in these nodes, more lymph nodes are removed. If no cancer is found, no further surgery is needed.
Axillary clearance is done when we know that cancer has already spread to the underarm lymph nodes. In this procedure, all the lymph nodes in that area are removed. It is done during the same surgery under the same anesthesia. After this surgery, a drain is placed under the skin to remove fluid from the wound. This drain stays for 7 to 10 days and is removed once the fluid reduces. The fluid may have a little blood in it, which is normal.
Cervix Cancer
What is cervix cancer and cervical cancer?
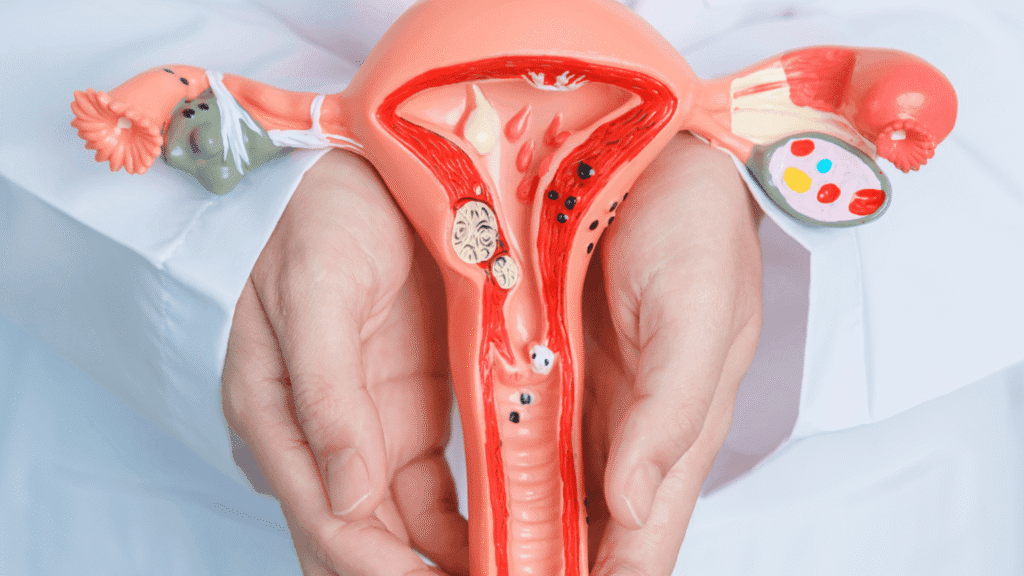
The cervix is the lower part of the uterus, also known as the neck of the womb. Both the uterus and cervix are part of a woman’s reproductive system. This system includes the vagina, uterus (womb) with the cervix, and ovaries. The cervix connects the womb to the vagina and acts as a strong muscle. It allows passage between these two parts. A diagram usually helps show where these organs are located inside the body.
Cervical cancer and its origin Cell types
The outer part of the cervix is covered with skin-like cells called the ectocervix. Inside the cervix, there are cells that make mucus, called glandular cells, and this area is known as the endocervix.
Sometimes, the skin-like cells on the outer surface can turn cancerous, causing squamous cell cervical cancer, which is the most common type. The glandular cells inside the cervix can also become cancerous, leading to adenocarcinoma of the cervix.
The transformation zone is the area where these changes usually happen. It’s located near the opening of the cervix, leading into a narrow passage called the endocervical canal, which connects the cervix to the womb.
During a cervical screening test, doctors or nurses check this transformation zone. This test does not look for cancer directly. Instead, it looks for abnormal cells that might turn into cancer if not treated in time.
How common it is?
Why have I developed cervical cancer?
Cervical cancer is more common in women under 45 years of age.
The main cause of cervical cancer is a long-lasting infection with certain types of HPV (Human Papillomavirus). HPV is a very common virus, and most people who are sexually active will get it at some point in their life. In most cases, the immune system clears the virus on its own and it doesn’t cause any problems.
Types of HPV
There are many types of HPV. Most are harmless, but some types can cause genital warts, and others can lead to changes in the body that may turn into cancer. Besides cervical cancer, HPV can also cause anal, vaginal, vulval, penile, and some mouth and throat cancers. HPV spreads through close skin-to-skin contact, usually during sex. Around 12 types of HPV are known to be high-risk for cervical cancer. Two of these types are responsible for about 70% of all cervical cancer cases.
Most people’s immune systems clear the virus within two years. But if the infection stays in the body for a long time, especially if it’s a high-risk type, the chances of getting cervical cancer go up.
Sex and Protection
Using condoms and practicing safer sex can help reduce the risk of getting HPV or passing it on. But condoms don’t give full protection. Still, safer sex also helps prevent other sexually transmitted infections (STIs).
HPV Vaccines
There are vaccines available to protect against HPV. Girls under 16 and women who haven’t had sexual activity are good candidates for the vaccine. In some countries, this vaccine is part of the regular health program. The vaccine protects against the main types of HPV that cause cervical cancer. But since it doesn’t protect against all types, it’s still important to get regular cervical screening even after getting the vaccine.
HIV and Other STIs
Women with HIV or AIDS have a higher risk of developing cervical cancer. Treatment for HIV may help lower that risk. Having another STI like chlamydia along with HPV can also raise the chances of getting cervical cancer.
Smoking
Smoking increases your risk of cervical cancer. The earlier you start and the more you smoke, the higher the risk. Smoking also makes it harder to treat abnormal cells in the cervix. It’s never too late to quit smoking — the sooner you stop, the better it is for your health.
Contraceptive Pill
About 1 in 10 cases of cervical cancer are linked to long-term use of the contraceptive pill. Taking the pill for more than 5 years can increase the risk, but this risk starts to drop after you stop using it. After 10 years, the risk is about the same as someone who never took the pill. The pill may slightly increase the risk of breast cancer, but it also reduces the risk of womb and ovarian cancers.
What are the symptoms?
Possible signs of cervical cancer include:
Light bleeding or spotting between periods
Periods that last longer or are heavier than normal
Bleeding after sex, pelvic exam, or douching
More vaginal discharge than usual
Pain during sex
Bleeding after menopause
Ongoing pain in the lower belly or back without a clear reason
Let me know if you’d like this in FAQ format or for a brochure.
What are the types of cervical cancer?
There are various types of cervical cancer. The most common one is squamous cell carcinoma. Cancer cells are grouped into three different grades based on how they look and grow.
At what stage is cancer?
The stage of cervical cancer shows how large the cancer is and whether it has spread. The type refers to the kind of cell where the cancer began.
Stage 1 means the cancer is only in the cervix.
Stage 2 means it has moved outside the cervix into nearby tissues.
Stage 3 means the cancer has spread to surrounding areas and lymph nodes in the lower belly.
Stage 4 means the cancer has spread to other parts of the body.
What treatment is needed?
Your treatment will depend on where the cancer is in the cervix, how big it is, whether it has spread to other parts of the body, and your overall health. Most people are treated with surgery or a mix of chemotherapy and radiotherapy (called chemo-radiotherapy).
How treatment is decided
Your doctor will look at your condition and then decide which treatment is best for you. There are different treatment options available depending on your case.
Surgery
Surgery is one of the main ways to treat cervical cancer. You may need a procedure called a radical hysterectomy. Your doctor will explain what happens before and after the operation.
Chemo-radiotherapy
This treatment combines chemotherapy and radiotherapy. Both are given together to treat the cancer.
Radiotherapy
You will first go through a planning session before starting radiotherapy. The medical team will explain how it works and what side effects may happen.
Chemotherapy
Chemotherapy uses special medicines to kill cancer cells. Your doctor will guide you on when and how you’ll get this treatment for cervical cancer.
What kind of surgery is done for cervical cancer?
Surgery is one of the main treatments for cervical cancer. Two types of surgeries are commonly used — radical hysterectomy and radical trachelectomy. Your doctor will explain what will happen before and after your surgery.
For early-stage cervical cancer, the usual treatment is to remove the womb completely (this is called a hysterectomy), or to give pelvic radiotherapy along with chemotherapy. These treatments usually mean that a woman cannot get pregnant or carry a baby in the future.
Radical trachelectomy is a different kind of surgery that removes only the cervix but keeps the uterus (womb) in place. This option can allow women to become pregnant and have children later. However, it is only suitable for women with very small cancers that are limited to the cervix.
This surgery is done by highly trained cancer doctors in only a few special hospitals around the world. If the cancer is less than 2cm, the trachelectomy can be done through the vagina. If it’s less than 4cm, it might be done through the abdomen, but more research is still needed for this method.
A radical hysterectomy means removing the womb, cervix, some nearby tissues, the top part of the vagina, lymph nodes in the pelvic area, and sometimes the fallopian tubes and ovaries. The most reliable way to do this surgery is through open surgery, which means making a cut on the tummy. Studies show this method gives better survival chances. You can also ask your surgeon about keyhole surgeries (laparoscopic or robotic) to see if they are right for you.

Stomach Cancer
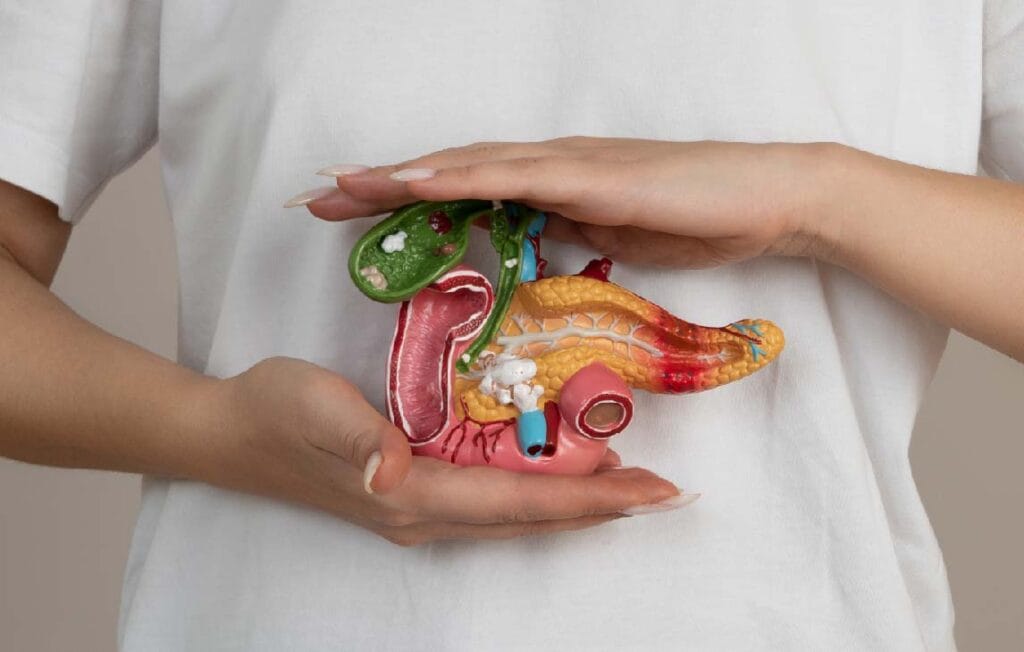
What is stomach? Where is it located?
The stomach is a bag-like organ made of muscle. It is part of the digestive system and is located on the upper left side of the belly, between the food pipe (esophagus) and the small intestine. The stomach makes acid and special juices to help break down food. This process happens in the first 2 to 4 hours after you eat.
During this time, the food is broken down into smaller parts. The stomach muscles move and churn the food to make digestion easier. Once the food is soft and broken down, it is pushed into the small intestine.
The stomach is close to other important organs like the liver, pancreas and spleen. The stomach itself has three main parts. Cancer can grow in any one of these parts or in more than one. The type of surgery needed depends on where the cancer is growing inside the stomach.
Are there different types of stomach cancer?
There are different types of stomach cancer. The most common type is called adenocarcinoma. Around 90 to 95 out of every 100 people with stomach cancer have this type.
Some other less common types of stomach cancer include:
Gastrointestinal stromal tumor (GIST)
Neuroendocrine tumors (also called carcinoid tumors)
Primary gastric lymphoma
Leiomyoma
Each type of stomach cancer is different and may need a different treatment plan.
What are the risk factors?
The exact cause of stomach cancer is not fully known. It usually happens due to a mix of different factors, not just one. Some things that may increase the risk include an unhealthy diet, infection from a bacteria called Helicobacter pylori (H. pylori), smoking, and having acid reflux for a long time.
Eating too much salty, pickled, or smoked food, as well as dried fish, meat, or refined carbs, can raise the chances of getting stomach cancer. But some people may still get this cancer even if they don’t have any of these risk factors.
In rare cases, stomach cancer can run in families. If a close family member (like a parent or sibling) had stomach cancer, your chances may be higher.
What are the symptoms of stomach cancer?
The exact cause of stomach cancer is not fully known. It usually happens due to a mix of different factors, not just one. Some things that may increase the risk include an unhealthy diet, infection from a bacteria called Helicobacter pylori (H. pylori), smoking, and having acid reflux for a long time.
Eating too much salty, pickled, or smoked food, as well as dried fish, meat, or refined carbs, can raise the chances of getting stomach cancer. But some people may still get this cancer even if they don’t have any of these risk factors.
In rare cases, stomach cancer can run in families. If a close family member (like a parent or sibling) had stomach cancer, your chances may be higher.
What Investigations will I be subjected to?
The first test usually done to check for stomach cancer is an upper endoscopy. In this test, the doctor looks inside the food pipe, stomach, and the first part of the small intestine using a thin, flexible tube. If they see anything unusual, they may take a small sample of tissue (called a biopsy) to check for cancer.
Next, a CT scan or a PET-CT scan of the chest, stomach area, and pelvis is done. This helps the doctor see if the cancer is only in the stomach or if it has spread to other parts of the body or lymph nodes.
A blood test called a complete blood count (CBC) is also done. Along with this, some special blood tests called tumour markers are checked. These give a starting point and will be repeated later to see how well the treatment is working and to monitor for any return of the cancer.
Other tests like lung function tests may also be done to make sure the patient is fit enough for anaesthesia and surgery if needed.
At what stage is my cancer?
Staging helps doctors understand how serious the stomach cancer is and what treatment will work best. It is based on test reports and scan results. Stomach cancer is divided into these stages:
Stage 1 (Early stage) – The cancer is only inside the stomach and has not spread outside.
Stage 2 and Stage 3 (Locally advanced stage) – The cancer is bigger, may have reached nearby organs, or spread to nearby lymph nodes.
Stage 4 (Advanced stage) – The cancer has spread to far parts of the body like the liver, lungs, or other organs.
What are my treatment options when I have been diagnosed with stomach cancer?
Treating stomach cancer needs a team of doctors. This team may include stomach specialists (gastroenterologists), cancer medicine doctors (medical oncologists), cancer surgeons (surgical oncologists), radiation experts, and diet experts (nutritionists).
The treatment plan depends on many things like the stage of cancer, tumor size, type of stomach cancer, whether it has spread, patient’s symptoms, age, and overall health.
In India, most patients are in stage 2 or 3 when they are diagnosed. So, chemotherapy is usually given first to shrink the tumor. After that, surgery is done to remove the cancer. Then another round of chemotherapy is given to make sure cancer does not come back.
If the cancer has already spread (metastatic stage), chemotherapy and HIPEC (a special heated chemotherapy treatment inside the abdomen) are used. Radiation therapy may also be used along with chemotherapy. This combination is called chemoradiation and can be given before or after surgery. In some advanced cancer cases, radiation is used to reduce pain, bleeding, or vomiting.
The final treatment plan is made carefully by the doctors, based on the patient’s condition.
Which kind of surgery is done for stomach cancer?
The type of surgery and how much needs to be removed depends on the stage and type of stomach cancer. In very early-stage cases, doctors may remove the cancer using a tube called an endoscope. But in India, stomach cancer is usually not found this early, so this type of surgery is rarely done.
For most patients, if the cancer is only in the stomach and nearby lymph nodes, the surgeon removes part of the stomach along with the tumor. This is called a subtotal or partial gastrectomy.
If the cancer is in the upper part of the stomach, a small part of the food pipe (oesophagus) may also be removed.
If it is in the lower part, then a small part of the upper intestine (duodenum) might be removed too.
If the cancer has spread throughout the stomach, then the whole stomach and some nearby tissues are removed. This is called a total gastrectomy. In this surgery, the food pipe is directly connected to the intestine so food can still pass through the body.
Along with the stomach, nearby lymph nodes are also removed. This is called lymph node dissection and is a normal part of stomach cancer surgery.
These surgeries can be done through open surgery or through small cuts using robotic or laparoscopic (keyhole) methods. The doctor will decide the best option based on the patient’s condition.
If the cancer has spread but only a little, surgery may still be possible. This can be combined with a special treatment called HIPEC (heated chemotherapy given inside the belly). Before this, doctors will check the cancer spread using a small camera through a process called laparoscopy. If the spread is very small, surgery with HIPEC may be done.
How do I prepare myself for surgery?
The preparation for stomach cancer surgery is similar to other major surgeries. If you smoke, it is very important to stop immediately. You should also start doing breathing exercises using a device called an incentive spirometer. Follow all the advice given by your heart doctor (cardiologist) and the doctor who gives anesthesia (anesthetist). Eating a high-protein diet is also helpful to improve your overall strength and nutrition before the surgery.
How major is the surgery? What are the possible complications?
Gastrectomy with lymph node removal is a major surgery and can have some risks. About 4 to 10 out of 100 people may face complications, and the risk of death is very low (less than 2%).
Some common problems that can happen after surgery include:
Leakage from the area where the surgeon joined two parts of the stomach or intestines (called anastomosis leak)
Bleeding after the surgery
Vomiting for a long time or a delay in passing stools
Your medical team will watch you closely and manage any issues if they happen.
Will I need further treatment after surgery?
After surgery, the doctor will decide if more treatment is needed. This decision depends on the final biopsy report, which usually takes around 7 to 10 days.
If the report shows that cancer has spread to any lymph nodes and the patient is fit enough, then further treatment may be advised.
What will be my survival after surgery? Are there any chances of the cancer coming back?
The survival depends on how early or late the cancer is found. On average, about 35 out of 100 people live for five years after successful surgery for stomach cancer.
Right now, there is no sure way to know who will be completely cured and who might have the cancer come back later.
Lung Cancer
What is lung? Where is it located?
The lungs help us breathe by taking in oxygen and removing carbon dioxide from the body. Our breathing system includes the windpipe (trachea), air tubes (bronchi), lungs, chest muscles, and diaphragm. Normally, we breathe 12 to 18 times every minute. The lungs are safely placed inside the chest area and take up most of the space there. In India, lung cancer is now becoming one of the most common types of cancer
What causes lung cancer?
Lung cancer does not happen because of just one reason. There are some risk factors that can increase the chances of getting lung cancer. These include:
Smoking, which is one of the biggest risks
Being around people who smoke (passive smoking)
Having a family member with lung cancer
Having had cancers in the head or neck before
Getting radiation on the chest for earlier illnesses like breast cancer or Hodgkin’s disease
Being exposed to chemicals or industrial pollution
Breathing polluted air
Having certain inherited health problems
But sometimes, people can still get lung cancer even if they don’t have any of these risk factors.
What are the symptoms of lung cancers?
The signs of lung cancer depend on where the tumour is located. You should visit a doctor if you notice any of the following:
Cough that lasts for more than two weeks
Blood in the spit (either bright red or dark)
Pain in the chest
Difficulty in breathing
Sudden weight loss without any clear reason
Feeling very tired all the time
Pain in other parts of the body (if the cancer has spread)
In Southeast Asia, because lung cancer is more common, people above 55 years old — especially those who smoke or have smoked — are advised to get a low-dose CT scan of the chest to check for any signs of cancer. Based on the results, doctors decide the next steps.
In India, there is no national screening program yet. But it is still a good idea for people above 55, especially smokers, factory workers, or those with a family history of lung cancer, to ask their doctor about getting a low-dose CT scan.
What Investigations will I be subjected to?
To confirm lung cancer, doctors usually do a bronchoscopic biopsy if the tumour is located in the center of the lung. If it is in the outer part (periphery), a CT-guided biopsy is preferred.
A whole-body PET CT scan helps the doctor see the size of the tumour, how close it is to nearby organs, if the lymph nodes in the chest are affected, and whether the cancer has spread anywhere else.
In rare cases, if the cancer is a special type called neuroendocrine, a test called chromogranin B may be done.
Other supporting tests like:
Pulmonary function test
DLCO
Echo and ECG
Perfusion lung scan
These are done to check how well the lungs are working and to see if the patient is fit enough for surgery or chemotherapy, depending on the stage of the cancer.
Are there different types of lung cancer?
Yes, there are different types of lung cancer based on the kind of cells the cancer starts from. The most common type is called non-small cell lung cancer. Another common one is small cell lung cancer.
There are also some less common types like neuroendocrine cancer and sarcoma.
The type of lung cancer helps the doctor decide which treatment will work best.
How to stage cancer?
Doctors can find the exact stage of lung cancer only after surgery by checking the tissues under a microscope. Lung cancer is usually grouped into two main types – operable and inoperable.
It is called locally advanced when the tumour is big or has spread to nearby organs or lymph nodes.
It is called metastatic when the cancer has spread to other parts of the body like the bones, brain, liver or adrenal glands.
Now that I have been diagnosed to have lung cancer, how will I be treated?
There are different types of treatments available for lung cancer. The main ones include:
Surgery
Chemotherapy
Radiotherapy
Immunotherapy
Surgery is usually the best option for patients in the early stages of lung cancer. In some cases, even people with locally advanced cancer may go for surgery after getting chemotherapy and radiation. After surgery, some patients may still need chemotherapy or immunotherapy to remove any leftover cancer cells.
Chemotherapy uses strong medicines to kill cancer cells or stop them from growing.
Immunotherapy helps the body’s own immune system fight against cancer. It targets only the cancer cells and has fewer side effects.
Targeted therapy uses special medicines that attack only the cancer cells without harming normal ones.
Radiation therapy uses beams of radiation to kill the cancer cells.
Thanks to modern treatments, many of these therapies now come with fewer side effects than before.
Which kind of surgery is done for lung cancer?
The type of lung surgery depends on where the cancer is and how much it has spread. Some common types of surgery include:
Segmentectomy – only a small part of one lobe of the lung is removed
Lobectomy – one full lobe of the lung is removed
Pneumonectomy – the entire lung on either the right or left side is removed
Sleeve Resection – a special type of surgery where the damaged part is removed but most of the healthy lung is saved
Lymph Node Removal – the nearby lymph nodes in the chest are also removed to check if the cancer has spread
The goal of surgery is to remove as much of the cancer as possible while keeping the healthy part of the lung safe.
Are there any alternatives besides surgery?
How do I prepare myself for surgery?
Before the surgery, the preparation is almost the same as any big operation. If you smoke, you must stop smoking completely. You should start doing breathing exercises using a spirometer or football bladder. If you are taking any medicines, follow the anaesthetist’s instructions about whether to continue them. It is also good to eat a high-protein diet to keep your body strong and healthy before the surgery.
How major is surgery? What are the possible complications?

Ovarian Cancer
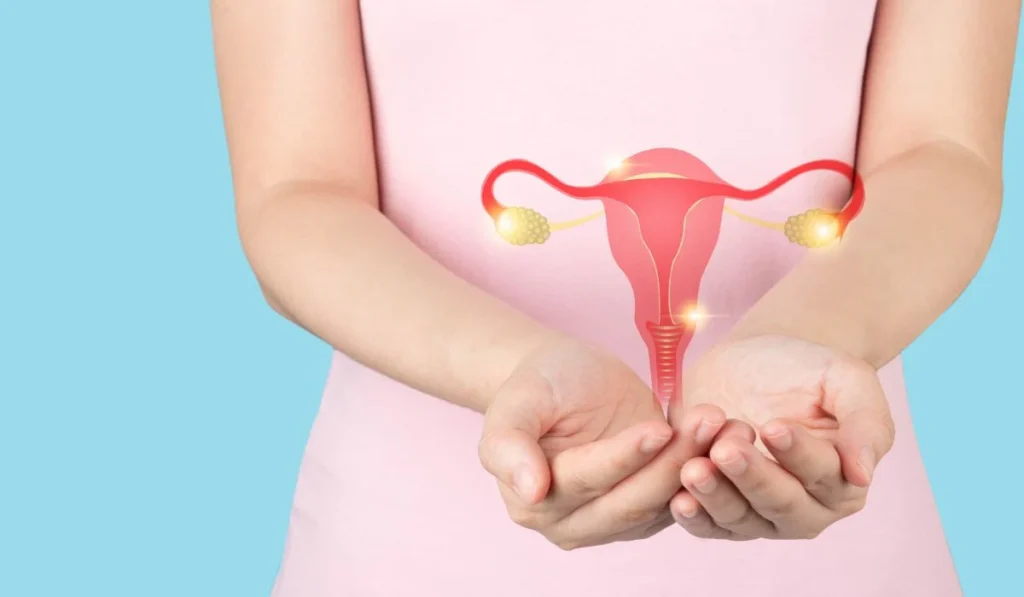
What are ovaries and ovarian cancer?
Ovarian hormones
Why have I developed ovarian cancer?
Possible risk factors for ovarian cancer.
1. Age:
Just like many other cancers, the risk of ovarian cancer goes up as women get older. Most cases are found in women who have already gone through menopause.
2. Inherited genes:
Most ovarian cancers happen because of gene changes that occur during a woman’s lifetime, not ones passed down from parents. But around 5 to 15 out of every 100 ovarian cancers happen because of inherited faulty genes. These include BRCA1 and BRCA2. These genes can also raise the chance of getting breast cancer. If anyone in your family has had ovarian or breast cancer, talk to your doctor. They can guide you on whether you need to see a genetics specialist.
3. History of breast cancer:
Women who had breast cancer, especially before the age of 40, may have a higher risk of ovarian cancer. This could be due to the same faulty genes.
4. Infertility or fertility treatment:
Some older studies showed a link between fertility drugs and ovarian cancer. But newer studies don’t support this clearly. It’s now believed that infertility itself may be the reason for the increased risk, not the treatments. More studies are going on to understand this better.
5. Endometriosis:
Women who have endometriosis may also have a slightly higher chance of developing ovarian cancer compared to those who don’t have it.
6. Smoking:
Smoking is linked to a higher risk of some types of ovarian cancer, especially mucinous ovarian cancer. The longer you smoke, the higher the risk becomes.
What are the symptoms?
These are some common signs that may be seen in women with ovarian cancer:
Feeling bloated or your stomach feeling swollen
Pain in the lower belly or pelvic area
Trouble eating or feeling full very quickly after starting to eat
Urge to urinate suddenly or needing to go to the toilet more often than usual
What investigations will I be subjected to?
What are the types of ovarian cancers?
There are different types of ovarian cancer. The most common one is called epithelial ovarian cancer. Some rare types include germ cell tumours, stromal tumours, and sarcomas. There is also a rare cancer called primary peritoneal cancer, which is treated just like epithelial ovarian cancer.
Epithelial ovarian cancer
This is the most common type. About 90 out of 100 ovarian cancers (90%) are epithelial.
Ovarian teratoma
This is a germ cell tumour. It usually affects young girls and women under 20. Cancerous types are rare.
Granulosa tumour
This is a type of stromal tumour. Only about 5 out of 100 women (5%) with ovarian cancer have this kind.
Primary peritoneal cancer
This is a rare cancer that starts in the lining of the tummy (peritoneum). It behaves like epithelial ovarian cancer and is treated the same way.
Fallopian tube cancer
This is also rare. It affects only about 1 out of 100 cases (1%) of female reproductive system cancers.
Borderline ovarian tumours
These are not actual cancers. They are abnormal cells found on the outer surface of the ovary. Usually, surgery can cure them completely.
At what stage is the cancer?
The stage of cancer means how big the cancer is and whether it has spread to other parts of the body. Knowing the stage helps the doctor choose the right treatment.
Stage 1 – The cancer is only in the ovary.
Stage 2 – The cancer has spread to the lower part of the tummy and nearby organs.
Stage 3 – The cancer has reached other parts of the abdomen, including the lymph nodes and upper tummy.
Stage 4 – The cancer has spread outside the tummy to other parts of the body, like the liver.
What treatment is needed?
The treatment for ovarian cancer depends on where the cancer is, how big it is, whether it has spread, and how healthy your body is overall. A team of doctors will work together to choose the best treatment plan for you.
How doctors decide your treatment:
Doctors look at the stage of the cancer and your health before choosing the treatment. You may have one or more of these treatments:
Surgery:
There are different types of surgery for ovarian cancer. It depends on the stage. Surgery is done in early cancer, when you have symptoms, or even in advanced cancer. The aim is to remove all or as much of the cancer as possible.
Chemotherapy:
Chemotherapy uses special medicines to kill cancer cells. It is often used for high-grade early cancers and advanced cancers. A chemotherapy doctor will explain how it works and the possible side effects.
Radiotherapy:
This treatment uses strong X-rays to kill cancer cells. It is not commonly used for ovarian cancer and is only given in rare cases.
What kind of surgery is done for ovarian cancer?
Surgery is usually done to remove a lump in the ovary and to confirm if it is cancer or not. It can also be done if doctors think the cancer has spread to other parts of the tummy.
During surgery, the doctor may remove the lump, one ovary or both ovaries. Sometimes, the uterus (womb), fallopian tubes and cervix are also removed. The part that is taken out may be quickly sent to the lab for testing to check if it looks like cancer.
If the doctor suspects cancer, they will also remove the fatty tissue in the tummy (called the omentum) and take samples from the nearby lymph nodes (pelvic and para-aortic glands) to check if the cancer has spread.
Some women may need bigger surgeries depending on how far the cancer has gone. This will be explained to you before surgery.
If the lump is small and has not spread, surgery can be done through a keyhole method. But if the lump is big or cancer has spread, the surgery is done by making a straight cut on the tummy.
The main goal of the surgery is to remove the lump or tumour safely, find out exactly what it is, and remove all the visible cancer if it has spread.
Pancreatic Cancer
After a pancreatoduodenectomy, what will happen to the functions these organs served?
The pancreas has two main jobs.
One part of it makes digestive juices that help break down food. The other part makes hormones like insulin, which helps control blood sugar. If the body doesn’t make enough insulin, it can lead to diabetes. In most cases, only the head of the pancreas is removed during surgery, so the rest of the pancreas usually continues to do its job.
The duodenum (the first part of the small intestine) mainly helps pass food from the stomach to the rest of the intestines. After surgery, new connections will be made using the small intestine so that food can still move through your digestive system normally.
I find my stools to be foul-smelled and bulky. Is it normal?
This condition is called steatorrhea. It means your body is not able to digest fats properly because there are not enough digestive juices from the pancreas. It can lead to loose, oily stools, a feeling of heaviness in the stomach, and weight loss.
Steatorrhea is not common after a pancreatoduodenectomy (Whipple surgery), but it can happen more often after removal of the whole pancreas.
Sometimes, even before cancer develops, the pancreas may not be working well due to other problems like pancreatitis. In such cases, steatorrhea can occur even after part of the pancreas is removed.
Treatment: This condition is usually managed by taking pancreatic enzyme supplements like Creon 10000 to 25000 units with meals, for lifelong use.
How would I know if I have developed diabetes following pancreatoduodenectomy?
Of late I have been losing weight. What is it likely due to?
Why do I experience burning sensation/pain in the upper abdomen?
This happens when bile, a digestive fluid, flows back into the stomach, causing irritation and discomfort. You may also vomit yellow-green fluid.
Treatment: Taking prokinetic medicines like Domperidone 10mg three times a day can help.
When can I start working again?
It is best to avoid lifting heavy weights for around three months after surgery to allow the scar to heal properly. If your job does not require hard physical work, you can return to work once you feel ready. Maintaining a healthy and active lifestyle is recommended. If you have a mostly inactive routine, activities like brisk walking at least three times a week are advised.
Can I resume sexual activities as before my illness?
Rectum Cancer
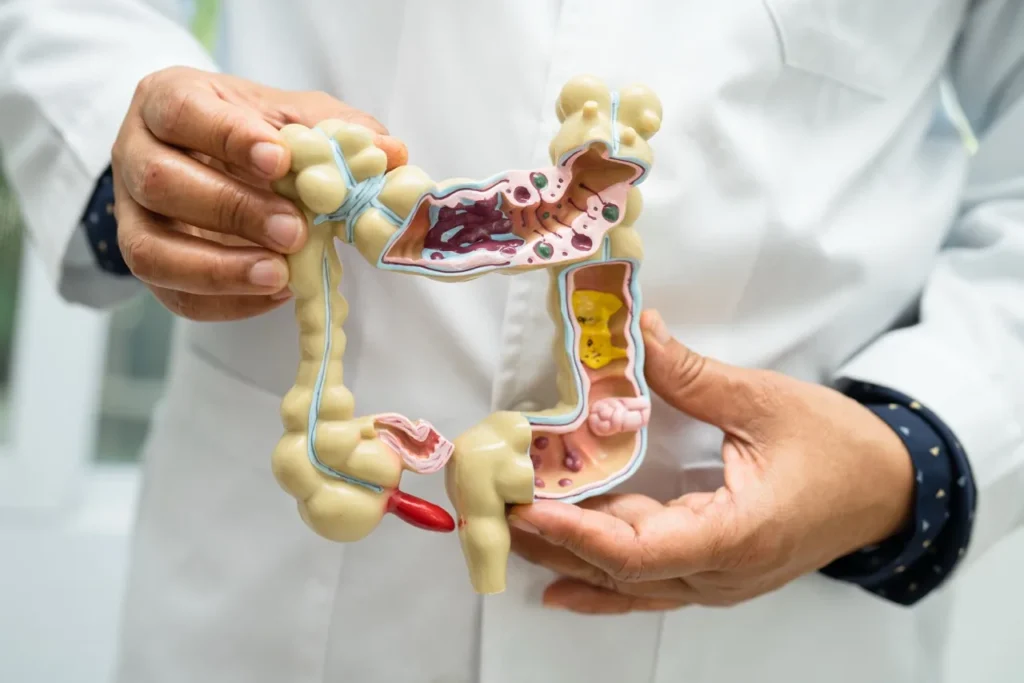
What is the rectum and what does it do?
The rectum is the last part of the large intestine or large bowel. It begins where the colon ends and leads to the short narrow passage called the anus. The large intestine is a long tube that makes up the final part of the digestive system. Partly digested food moves into the colon, where water is absorbed from it and turns it from liquid into solid. This solid waste is called stool or feces. The stool then moves into the rectum, the last section of the large intestine. The anal sphincter is a ring of muscle at the end of the anus that opens and closes to help control bowel movements. Cancer that starts in the rectum (rectal cancer) and cancer in the colon (colon cancer) are often grouped together and called “colorectal cancer.”
What are the risk factors?
The reasons why cancer develops are complicated, and rectal cancer cannot be linked to just one cause. Several factors may increase the risk of colon cancer.
Some of these risk factors include:
Getting older, eating a diet low in fiber and high in fat, living a sedentary lifestyle, having diabetes or obesity, smoking, and drinking alcohol.
Having had colorectal cancer or polyps before. If you have had colon cancer or pre-cancerous polyps, your risk of getting rectal cancer again is higher.
Having chronic inflammatory bowel diseases like ulcerative colitis or Crohn’s disease.
Inherited conditions like familial adenomatous polyposis (FAP) and Lynch syndrome (also called hereditary non-polyposis colorectal cancer or HNPCC) increase the risk.
Family history of colorectal cancer. If close family members have had colon or rectal cancer, your chances of getting it are higher, especially if more than one relative was affected.
Previous radiation therapy to the abdomen for other cancers can also raise the risk of colorectal cancer.
What are the symptoms of rectal cancer?
The symptoms of rectal cancer can be very similar to common conditions that are not cancer, like hemorrhoids (piles).
Signs and symptoms of colon cancer include a lasting change in your bowel habits, feeling like you cannot completely empty your bowel, diarrhea or constipation, or a change in the thickness of your stool. You might notice bleeding from the rectum, dark red or bright red blood in your stool, narrow stools, ongoing stomach discomfort such as cramps, gas, or pain, and unexplained weight loss.
What Investigations will I be subjected to?
The first test to diagnose rectal cancer is a colonoscopy or sigmoidoscopy. This exam lets doctors see the lower part of the digestive system, including the rectum and colon. If they find something unusual, they will take a small tissue sample (biopsy).
To find out the stage of the cancer, a CT scan or PET-CT of the chest and abdomen, along with an MRI of the pelvis, will be done. The MRI gives a clear picture of the muscles, organs, and other tissues around the tumor in the rectum. It also shows nearby lymph nodes and the different layers of the rectal wall. This helps the doctor understand if the tumor is only in the rectum or if it has spread to other places or lymph nodes.
A complete blood count and tumor marker tests will be done to get baseline results. These tests will be repeated later to check how well the treatment is working and for ongoing monitoring. Other tests, like lung function tests, may be done if needed to see if you are fit for anesthesia and surgery.
At what stage is my cancer?
Stage 1 (Early cancer) – Cancer is only in the rectum and has not spread beyond it.
Stage 2 and Stage 3 (Locally advanced cancer) – Cancer is bigger and may be invading nearby organs or has spread to lymph nodes.
Stage 4 (Metastatic cancer) – Cancer has spread to other distant parts of the body.
What are my treatment options when I have been diagnosed with rectal cancer?
Precise staging of the cancer is determined through histopathology and can be done after surgery. Lung cancer is generally divided into operable and inoperable locally advanced types—where the cancer is large and/or has invaded nearby organs or enlarged lymph nodes. Metastatic lung cancer refers to cancer that has spread to distant parts of the body, such as the bones, brain, liver, or adrenal glands.
Now that I have been diagnosed to have lung cancer, how will I be treated?
The exact treatment can vary depending on many factors such as the stage of the disease, size of the tumour, its distance from the anal sphincter, whether the cancer has spread, presence of symptoms, the patient’s age and overall health, and other considerations. For stage 1 cancer, surgery is usually the first option. For stages 2 and 3, treatment often begins with radiation combined with chemotherapy, followed by surgery. Sometimes, additional chemotherapy is given before surgery. After surgery, the decision to give further chemotherapy depends on the final pathology report. For stage 4 cancer, the initial treatment depends on how far the disease has spread. If there is bowel obstruction, a stoma may be created. A stoma is a surgical opening made in the abdominal wall to allow waste to exit if normal bowel movements are not possible. Radiation may also be used in metastatic cases to relieve symptoms like pain, vomiting, or bleeding causing severe anemia, and for metastases in the liver or other organs. The treatment plan will be personalized based on these factors.
Treating rectal cancer requires a coordinated team approach involving gastroenterologists, surgical oncologists, medical oncologists, radiation oncologists, and nutritionists.
What kind of surgery is done for rectal cancer?
The type of surgery and how much needs to be done depends on where the cancer is in the rectum and how far it has spread. If the cancer is found on a small polyp, doctors may remove it using a simple endoscopic procedure.
In most cases, when the cancer is only in the rectum and nearby lymph nodes and not too close to the anal opening, surgeons will remove the affected part of the rectum and nearby lymph nodes. Then, they join the remaining parts of the intestine. This is called anterior resection or low anterior resection.
If the cancer has reached the inner part of the muscles that help you control your bowel (called the anal sphincter), doctors will do a surgery called inter-sphincteric resection. In some cases, a temporary stoma may be made. A stoma is a small opening made on your stomach to allow waste to pass out of the body, giving time for the intestine to heal properly.
If the cancer has spread outside the rectum or both anal sphincters are affected, doctors may do a surgery called abdominoperineal resection. In this case, the stoma will be permanent. Your doctors will fully explain what each surgery means for you.
These surgeries can be done in two ways: either with a large open cut or using small cuts with the help of robotic or laparoscopic (keyhole) methods. The method will depend on your condition and what the surgeon finds best.
If the cancer has spread to the lining inside the belly, a major surgery called cytoreductive surgery is done along with a special chemotherapy treatment called HIPEC. If the cancer has spread to the liver, doctors may do surgery to remove cancer from both the rectum and the liver at the same time or in stages. Other treatments like radiofrequency, alcohol injection, microwave ablation or radiation may also be used for the liver.
If cancer has spread to any other part of the body, doctors may remove those parts as well along with the rectum.
How do I prepare myself for surgery?
Preparing for this surgery is similar to preparing for any major operation. If you smoke, it is best to stop right away. You will also be asked to do breathing exercises using a tool called an incentive spirometer, which helps improve your lung function before surgery.
You will need to follow the advice given by the heart doctor (cardiologist) and the anesthesia doctor (anesthetist). To keep your body strong for surgery, you should eat a high-protein diet to improve your nutrition.
One day before the surgery, you will be given a laxative to clean your stomach and intestines. This is known as bowel preparation and helps get your body ready for the operation.
How major is surgery? What are the possible complications?
Rectal surgery is a major operation and, like any big surgery, it can have some risks. Around 4 to 8 out of 100 people may face serious complications, and the chance of death is very low, less than 1%.
Some of the main problems that can happen after surgery include:
Leak at the joint where the two ends of the intestine are connected during surgery
Bleeding after the operation
Ongoing vomiting or delay in passing gas or stool after surgery
Your surgical team will closely monitor you to catch and manage any of these issues early.
How long will my recovery be after surgery?
How long will I stay in the hospital after surgery?
The number of days you stay in the hospital depends on how well you recover and the type of surgery you had. Most people stay for 2 to 4 days. Your surgical team will guide you and explain what to expect during your stay.
Will I need any treatment after surgery?
This depends on the final biopsy report from the surgery, which usually comes in 7 to 10 days. If the report shows that more treatment is needed, you may be advised to take further treatment (called adjuvant therapy), and your doctor will refer you to the right specialist for it.
Get in Touch Now
For any enquiry reach out to us today We are here to help you every step of the way