Rectum Cancer
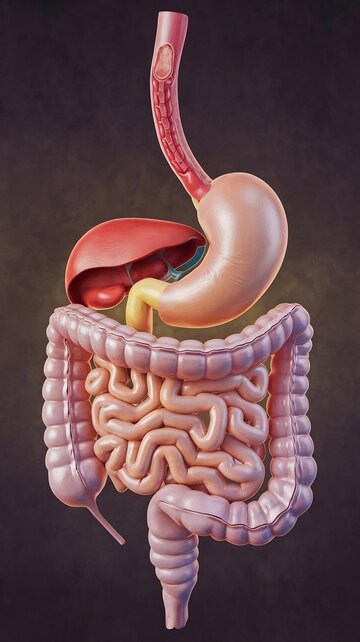
What is the rectum and what does it do?
The rectum is the last several inches of the large intestine, also known as large bowel. It starts at the end of the final segment of your colon and ends when it reaches the short narrow passage leading to the anus. The large intestine is a long tube-shaped organ that forms the last part of the digestive system. Partly digested food moves into the colon. In the colon, water is absorbed from unused food, changing it from liquid to a solid. This solid, unused food is called feces or stool. Stool then moves into the last section of the large intestine, called the rectum. Your anal sphincter is a ring of muscle that opens and closes at the bottom of your anus and plays a large role in controlling bowel function. Cancer inside the rectum (rectal cancer) and cancer inside the colon (colon cancer) are often referred to together as “colorectal cancer.”
What are the risk factors?
The reason why cancer develops is a complex question and the development of rectal cancer cannot be attributed to any single factor. There are multiple factors suggested that could be responsible for causing colon cancer.
Factors that may increase your risk of colon cancer include:
- Older age, low-fiber, high-fat diet, a sedentary lifestyle, diabetes, obesity, smoking, alcohol, are all risk factors for colon cancer.
- A personal history of colorectal cancer or polyps. If you’ve already had colon cancer or pre-cancerous colon polyps, you have a greater risk of rectal cancer in the future.
- Inflammatory intestinal conditions. Chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn’s disease can increase your risk of rectal cancer.
- There are a few inherited syndromes that increases colon cancer risk. They are familial adenomatous polyposis(FAP) and Lynch syndrome, which is also known as hereditary non-polyposis colorectal cancer (HNPCC).
- Family history of colorectal cancer. You’re more likely to develop rectal cancer if you have a blood relative who has had the disease. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
- Previous radiation therapy directed at the abdomen to treat previous cancers increases the risk of colorectal cancer.
What are the symptoms of rectal cancer?
The symptoms and signs of rectum can be the same as those of extremely common conditions that are not cancer, such as hemorrhoids (piles).
Signs and symptoms of colon cancer include a persistent change in your bowel habits and a feeling that your bowel doesn’t completely, diarrhea or constipation or a change in the consistency of your stool, rectal bleeding, dark maroon or bright red blood in stool, narrow stool, persistent abdominal discomfort, such as cramps, gas or pain, and unexplained weight loss.
What Investigations will I be subjected to?
The first investigation to diagnose stomach cancer is a colonscopy/sigmoidoscopy. This examination allows doctors to view the lower portion of the digestive tract including the rectum and colon. If an abnormality is seen, a sample of tissue (biopsy) will be removed. A computed tomography (CT) or a PET-CT of the chest, abdomen and an MRI of the pelvis will be done to determine the stage of the cancer. An MRI provides a detailed image of the muscles, organs and other tissues surrounding a tumour in the rectum. An MRI also shows the lymph nodes near the rectum and different layers of tissue in the rectal wall. This will give the physician an idea regarding the spread of the tumour – whether it is confined to the rectum or if it has spread to other organs or lymph nodes. A complete blood count is a standard blood test, along with which tumour markers will be done to get a baseline value. This will be repeated later to assess the response to treatment and for the surveillance. Other investigations like lung function tests will be done if required to assess the patient’s fitness for anaesthesia and surgery.
At what stage is my cancer?
Stage1(Early cancer) – Cancer within rectum and has not spread outside of it
Stage 2 and Stage 3 (Locally advanced cancer) – Cancer is large and/or invading neighbouring organs and/or spread to lymph nodes
Stage 4 (Metastatic cancer) – Cancer spread to distant organs
What are my treatment options when I have been diagnosed with rectal cancer?
Accurate staging of the cancer is based on histopathology and is possible after surgery. Lung cancer can be broadly classified into operable and inoperable locally advanced – when cancer appears large and or/ invading other surrounding organs, which enlarged lymph nodes. Metastatic – when cancer has spread far from the lung e.g. to the bone, brain, liver or adrenal gland.
Now that I have been diagnosed to have lung cancer, how will I be treated?
Specific treatment may vary, depending upon numerous factors, such as disease stage, tumour size, distance from the anal sphincter, whether the cancer has spread, the presence or absence of certain symptoms, an individual’s age and general health, and/or other elements. For stage1, surgery will most likely be the first treatment of choice. For stage2 and 3, radiation along with chemotherapy will most likely be the initial treatment followed by the surgery. Sometimes further chemotherapy will also be given before performing surgery. Following this, the need for chemotherapy after surgery will be decided on the final histopathology report. For stage 4 cancer, the first treatment will depend based on the extent of the disease; if the patient has bowel obstruction, a stoma would be performed. A stoma is an opening in your belly’s wall that a surgeon makes in order for waste to leave your body if you can’t have a bowel movement through your rectum. Sometimes radiation treatment is offered to metastatic cancer patients to decrease certain symptoms (pain, vomiting and bleeding causing severe anaemia) and for liver and other metastases. The appropriate sequence of treatment will be tailor-made based on the above-mentioned factors.
The treatment of rectal cancer requires the coordinated efforts of a team of gastroenterologists, surgical oncologists, medical oncologists, radiation oncologists and nutritionists.
What kind of surgery is done for rectal cancer?
The exact surgery and extent of surgery depends upon the part of the rectum involved and stage of the cancer. Surgery can include endoscopic resection, if the cancer is on a polyp.
For most when the cancer is confirmed to the rectum and adjacent lymph nodes and is away from the anal sphincter, surgeons need to remove a part of the rectum along with the lymph nodes and then join the remaining intestine. This is called as an anterior resection or low anterior resection of rectum. If the inner part of the anal sphincter complex is involved, a procedure called inter-sphincteric resection of rectum will be performed. A temporary stoma might be performed along with all the above-mentioned procedures. This is done so as to protect the newly formed joint between the intestines. As explained before, a stoma is an opening in your belly’s wall that a surgeon makes in order for waste to leave your body if you cant have a bowel movement through your rectum.
If the cancer has spread outside the rectum or it involves both the anal sphincters, then a procedure called abdominoperineal resection of rectum is performed. The stoma formed during this surgery will be a permanent one. Your surgical team will explain these procedures in detail.
These surgeries can be performed either as an open procedure or as robotic/laparoscopic (key-hole surgery). The appropriate procedure will be decided by the surgeons after considering certain factors.
If the disease has spread to the lining of the abdominal cavity, an extensive surgery called cytoreductive surgery along with HIPEC (hyperthermic intraperitoneal chemotherapy) would be offered. If the disease has spread to liver, surgery will be performed to remove the disease on the colon and liver either during the same sitting or as a staged process. Other forms of treatment can also be offered for liver like radiofrequency ablation, alcohol ablation, microablation and radiation. Spread of disease to any other organ will be removed along with the rectum.
How do I prepare myself for surgery?
The preparation is the same as for any major surgery. If you are a smoker, immediate cessation is advisable. Breathing exercise using incentive spirometry should be started. Cardiologists’ and anesthetists’ advice needs to be followed. A high protein diet is preferred to improve nutrition. A bowel preparation with a laxative would be performed on the day before surgery.
How major is surgery? What are the possible complications?
Rectal surgery is a major surgery with a risk of major complications (4-8%) and a very small risk of death (<1%). The major complications of the surgery are:
- Leak of anastomosis (the surgical connection between the two ends of intestine)
- Post-operative bleeding
- Prolong vomiting/Delayed passing of stools
How long will my recovery be after surgery?
The duration of hospital stay after your surgery depends on your recovery and the type of surgery you had. Most patients stay in the hospital for 2-4 days. Your surgical team will explain in detail what to expect.
Will I need further treatment after surgery?
The decision about adjuvant treatment is based on the final histopathology report which will be available in approx. 7-10 days. If required, you may be referred for adjuvant.