Stomach Cancer
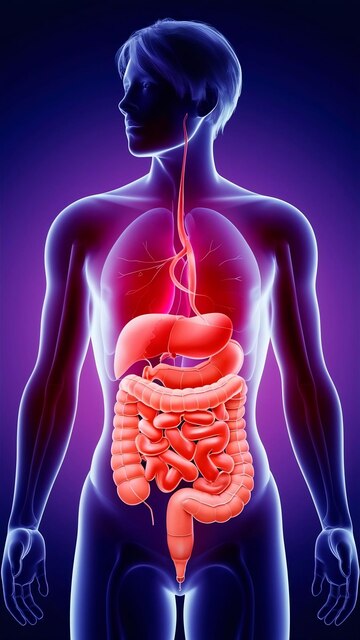
What is stomach? Where is it located?
The stomach is a muscular bag-like organ of the digestive system located on the left side of upper abdomen between the oesophagus (food pipe) and the small intestine. The stomach secretes acid and enzymes that digest food, for the first 2-4 hrs after eating. In these hours, the food is broken down, followed by the stomach muscles contracting periodically and churning the food to enhance digestion and propel the smaller pieces of food in to the small intestine. The major organs that surround the stomach are the liver, pancreas and spleen. The stomach is sub-divided into three parts (as shown in the figure) and cancer may affect one or more parts. The type of surgery will depend on the location of the tumour.
Are there different types of stomach cancer?
There are several different forms of stomach cancer. The most common is called adenocarcinoma, which accounts for about 90-95% of people with stomach cancer. Other types include gastrointestinal stromal tumor (GIST), neuroendocrine (carcinoid) tumors, primary gastric lymphoma, and leiomyoma.
What are the risk factors?
The reason why cancer develops is a complex question and the development of stomach cancer cannot be attributed to any single factor. There are multiple factors suggested that could be responsible for causing stomach cancer. These include diet, Helicobacter pylori (H.pylori) infection, smoking, and long-term gastric reflux. High intake of salted, pickled or smoked foods, as well as dried fish, meat and refined carbohydrates significantly increase the risk of developing stomach cancer. However, patients may develop these cancers even without any of these factors being present. In rare instances, stomach cancer can run in families. Having a first-degree relative with stomach cancer is considered a risk factor for the disease.
What are the symptoms of stomach cancer?
The symptoms of stomach cancer can vary greatly from one person to another and depends on the exact location of the tumour. In general, there are no symptoms in the early stages (asymptomatic). Some of the symptoms associated with the cancer are feeling full after eating a small amount of food (early satiety), feeling bloated after eating, loss of appetite, unintended weight loss, heart-burns, difficulty in swallowing and vomiting (if associated with other symptoms). Unexplained anaemia, causing fatigue, paleness of skin, and shortness of breath is a form of presentation and hence such patients need to undergo endoscopy to rule out stomach cancer. Patients who present with heart-burns and reflux for the first time after the age of 40 years need to undergo an endoscopy to rule out stomach cancer amongst other causes. Lump in the abdomen and back pain are late signs of the disease and usually indicate an advanced disease.
What Investigations will I be subjected to?
The first investigation to diagnose stomach cancer is an upper endoscopy. This examination allows doctors to view the upper portion of the digestive tract including the oesophagus, stomach, and the duodenum. If an abnormal is seen, a sample of tissue (biopsy) will be removed. A computed tomography (CT) or a PET-CT of the chest, abdomen and pelvis will need to be performed to determine the stage of the cancer. This will give the physician an idea regarding the spread of the tumour – whether it is confined to the stomach or if it has spread to other organs or lymph
nodes. A complete blood count is a standard blood test, along with which tumour markers will be done to get a baseline value. This will be repeated later to assess the response to treatment and for surveillance. Other investigations like lung function tests will be done if required to assess the patient’s fitness for anaesthesia and surgery.
At what stage is my cancer?
Staging is important to help characterise the potential disease course and determine appropriate treatment approaches. Based on clinical and radiological findings, stomach cancer can be grouped into:
Stage 1 (Early cancer) – Cancer within stomach and with no spread outside of it
Stage 2 and Stage 3 (Locally advanced cancer) – Cancer is large and/or invading neighbouring organs and/or spread to lymph nodes
Stage 4 (Metastatic cancer) – Cancer spread to distant organs.
What are my treatment options when I have been diagnosed with stomach cancer?
Stomach cancer treatment requires the coordinated efforts of a team of medical professionals, such as gastroenterologists, medical oncologists, surgical oncologists, radiation oncologists, and nutritionists.
Specific treatment may vary, depending upon numerous factors, such as disease stage, tumour size, specific stomach cancer subtype, whether the cancer has spread, the presence or absence of certain symptoms, an individual & age and general health, and/or other elements. In India, as most of the stomach (adenocarcinoma) cancer patients belong to stage 2 and stage 3, chemotherapy will be given first so as to downstage the disease. This will be followed by surgery, which is the main curative option for stomach cancer, followed by further course of chemotherapy. For metastatic patients, chemotherapy and HIPEC (hyperthermic intraperitoneal chemotherapy) are treatment options. Radiation therapy may also be used before and after surgery and is given along with chemotherapy (called as chemoradiation). Sometimes radiation treatment is offered to metastatic cancer patients to decrease certain symptoms (pain, vomiting, and bleeding causing severe anaemia). The appropriate sequence of treatment will be tailor-made based on the above mentioned factors.
Which kind of surgery is done for stomach cancer?
The exact surgery and extent of surgery depends upon the type and stage of the cancer. Surgery can include endoscopic resection, in very early-stage cancer. Stomach cancer in India is rarely diagnosed in very early stage so as to allow for endoscopic resection.
For most patients with gastric cancer confined to the stomach and adjacent lymph nodes, surgeons need to remove some of the stomach along with the tumour. This is called a subtotal (partial) gastrectomy. If the cancer is in the upper part of the stomach, sometimes some of the oesophagus may also need to be removed. If the cancer is in the lower part of the stomach, sometimes some of the upper portion of the lower intestines called the duodenum may need to be removed. Sometimes, surgeons must remove the entire stomach and some of the surrounding tissue. This is called a total gastrectomy. It is most often recommended when cancer has spread throughout the stomach. During this surgery, the end of the oesophagus is connected directly to the duodenum to allow for the passage of food.
A common part of the surgery called as lymph node dissection is performed to remove adjacent lymph nodes.
These surgeries can be performed either as an open procedure or as
robotic/laparoscopic (key hole surgery). The appropriate procedure will be decided by the surgeons after considering certain factors.
If the patient has metastatic disease with minimal spread to organs, surgery can still be considered, along with HIPEC (hyperthermic intraperitoneal chemotherapy). This option will be offered after staging the disease laparoscopically and confirming the minimal spread to organs.
How do I prepare myself for surgery?
The preparation is the same as for any major surgery. If you are a smoker, immediate cessation is advisable. Breathing exercised using incentive spirometry should be started. Cardiologists and anaesthetists advise needs to be followed. A high protein diet is preferred to improve nutrition.
How major is the surgery? What are the possible complications?
Gastrectomy with lymaphadenectomy is a major surgery with a risk of complications (4-10%) and a very small risk of death (<2%). The major complications of the surgery are-
- Leak of anastomosis
- Post-operative bleeding
- Prolong vomiting/Delayed passing of stools
Will I need further treatment after surgery?
The decision about adjuvant treatment is based on the final histopathology report which will be available in approximately 7-10 days. If any of the lymph nodes are positive and the performance status is good enough, then you may be referred for adjuvant treatment.
What will be my survival after surgery? Are there any chances of the cancer coming back?
The survival depends on the stage of the disease. The average five year survival after curative surgery is around 35%. This means that around 35 out of 100 patients with stomach cancer will survive at the end of five years. As of now there is no fool- proof way of predicting which patients will have recurrence and who will not.